What Are Hives?
Hives, also known as urticaria, involve an itching sensation and swollen, red marks. The itching may be mild to severe, depending on the case. Hives are due to an increase in body temperature with sweating, exercise, hot showers, and/or anxiety. Try not to scratch, drink alcoholic beverages, exercise, and get emotionally stressed, as these may worsen the itching.
Symptoms of hives can last for different amounts of time. There are 2 types of hives:
- Acute urticaria: hives that last six weeks or less
- Chronic urticaria: hives that last or recur for more than six weeks
In general, the causes of acute and chronic hives vary.
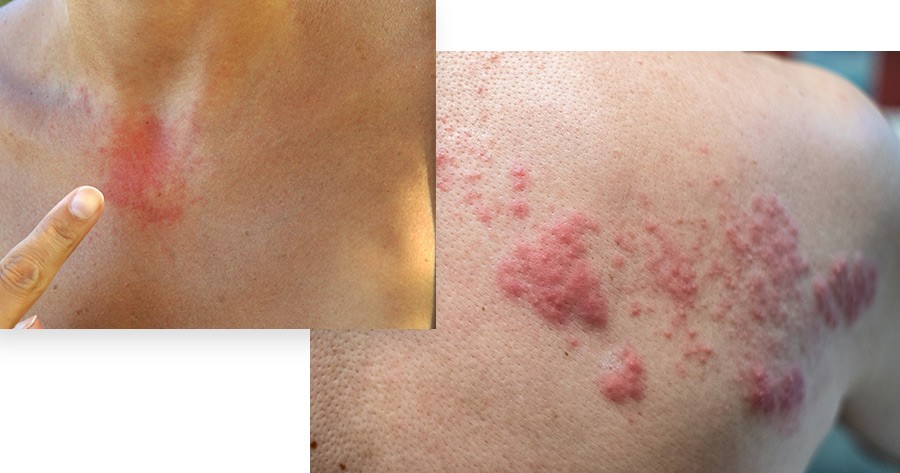
Hives are raised red or white welts that vary in size; appear anywhere on the body (including inside the mouth); cover all or parts of the body; cause itching, burning or stinging; while each individual hive does not last more than 24 hours, the condition can last from a few hours to six weeks (acute) or longer than six weeks (chronic). According to Dr. Fox, “they are rarely life threatening, requiring immediate medical attention, particularly when they cause swelling in the throat. Fortunately hives are typically treatable.”
In non-emergent situations, a dermatologist can work closely with a patient to determine if the hives are caused by food (milk, soy, eggs, nuts, shellfish and wheat are top culprits, along with additives and preservatives), medications (pain killers, antibiotics and blood pressure medications in particular), external stressors (exercise, water, sun exposure and extreme temperatures), and internal stressors (infection, illness and autoimmune disorders, liver disease, and allergic reaction to donor blood). Hives will sometimes disappear on their own without treatment, but when they don’t, dermatologists can help patients find the right medication or combination of medications to treat the condition.

What Causes Hives?
Acute hives
last six weeks or less and are generally caused by one of the following:
- Foods such as peanuts, eggs, nuts and shellfish
- Medications such as aspirin and antibiotics (especially penicillin and sulfa)
- Stings or bites
- Blood transfusions
- Infections including a cold, urinary tract infection, strep throat, infectious mononucleosis and hepatitis, among others
Generally, the hives go away when the cause is avoided, removed or treated.
Chronic hives
last for more than six weeks. The cause of chronic hives is unknown although the immune system is often involved. In other cases, chronic hives may be associated with thyroid disease or other hormonal imbalances. In most cases, chronic hives gradually disappears. “Physical urticaria,” a type of chronic hives in which hives can have one or more physical cause may include:
- Rubbing or scratching. The most common reason for chronic hives, these physical hives appear in the area of rubbing or scratching for less than an hour.
- Change in temperature. Hives can be caused by heat or cold, usually by exposure to low temperature followed by re-warming. This can be severe if there is a general body cooling, for example after jumping into a swimming pool.
- Constant pressure. Hives can also come in the form of red swelling caused by constrictive clothing such as belts. In some occupations they occur in parts of the body under constant pressure, such as hands in carpenters.
- Sun exposure. Hives may occur within a few minutes after exposure to the sun.
- Inflammation of the blood vessels, called vasculitis, can also cause hives. These hives are less itchy and more painful, and may leave a bruise on the skin.
How are the causes of hives identified?
Sometimes it is obvious – a person eats peanuts or shrimp, and then develops hives within a short time. In some cases, the cause cannot be identified. If the hives involve swelling of the tongue or trouble breathing, immediately go to the emergency room to be evaluated.
If a food allergy is suspected, it can be extremely helpful to jot down a diary of foods eaten before the hives started.
Chronic hives should be evaluated by an allergist. The allergy specialist will take your detailed medical history, including exposures from your work and home environment, and current and recent medications. The allergist will examine you for possible causes of hives with a skin, blood, or urine test.
The exact cause of chronic hives can be identified in about 20% of cases, although research is still being done to identify more causes and more effective treatments for hives.


Hives, in most cases, are treated with antihistamines. They are effective, long-lasting and have minimal side effects. Severe cases may require temporary treatment with prednisone, a similar corticosteroid medication or immune modulator.
If the rash involves swelling of the tongue or lips, or you have trouble breathing, an epinephrine self-injector will be prescribed to carry with you at all times.
If the cause of hives can be identified, the best treatment is to avoid or eliminate it. For example:
- Foods – If a problem with a specific food is strongly suspected, you should not eat that food. Read packaged food labels and question restaurant staff about ingredients in your dish.
- Rubbing or scratching – Avoid harsh soaps and tight clothing. Frequent bathing may increase the problem of dry skin, which leads to scratching, further aggravating the condition.
- Constant pressure – Loose-fitting clothing will help relieve hives caused by pressure.
- Change in temperature – If your hives are caused by cold, you should not swim alone. If you get severe cases, you should not swim at all. Try avoiding exposure to cold, and wear warm clothing to avoid getting hives.
- Sun exposure – Wear protective clothing and apply sun block when outdoors.
- Medications – If a specific medication gives you problems, stop taking it and notify your doctor and pharmacist.
Treating Hives
Antihistamines work to control symptoms by blocking the body’s release of histamines in response to an allergen. There are newer (second generation) and older (first generation) antihistamines, prescription and over-the-counter, and sometimes a combination will give the patient the best results. Antihistamines don’t treat the cause, only the symptoms.
Second-generation antihistamines are usually attempted first, since they are typically as effective as first-generation antihistamines, and better tolerated as they generally cause minimal sedation or tiredness. Some examples are Loratadine (Claritin, Alavert), Fexofenadine (Allegra), Cetirizine (Zyrtec), Levocetirizine (Xyzal) and Desloratadine (Clarinex).
First-generation antihistamines may be prescribed when non-sedating second-generation drugs don’t work. Because these drugs can cause drowsiness, and impair one’s ability, they are often taken before bedtime. Examples include Hydroxyzine (Vistaril), Diphenhydramine (Benadryl) and Chlorpheniramine (Chlor-Trimeton).
When antihistamines don’t relieve symptoms:
H-2 antagonists. Cimetidine (Tagamet), ranitidine (Zantac), nizatidine (Axid) and famotidine (Pepcid AC) are sometimes used with antihistamines, but can cause side effects ranging from gastrointestinal problems to headache.
Corticosteroids. While topical corticosteroids are typically ineffective, oral corticosteroids such as prednisone can provide relief from the uncomfortable symptoms of severe hives by reducing swelling, redness and itching, but can’t be taken long term due because of the serious side effects they occasionally cause, such as weakening the immune system. Often the hives may return when stopping the corticosteroids.
Tricyclic antidepressants. Doxepin’s (Zonalon) antihistamine properties can relieve itching, but they also cause dizziness or drowsiness and other side effects.
When a physical or systemic cause is not evident, and indicators point to stress as a possible cause for hives, it’s still important to confer with a dermatologist. “Desperation may lead a patient to try anything and everything to cure hives,” said Dr. Fox, “but with guidance from a dermatologist, a patient can instead approach the process in a systematic fashion.”
Researchers are currently studying if hives can be lessened by hypnosis and other relaxation techniques; hypnosis has been shown to help patients suffering from psoriasis, warts and hair loss, and meditation, biofeedback and talk therapy have been shown to help psoriasis.
