Spider Vein Treatment & Removal
What Are Spider Veins?
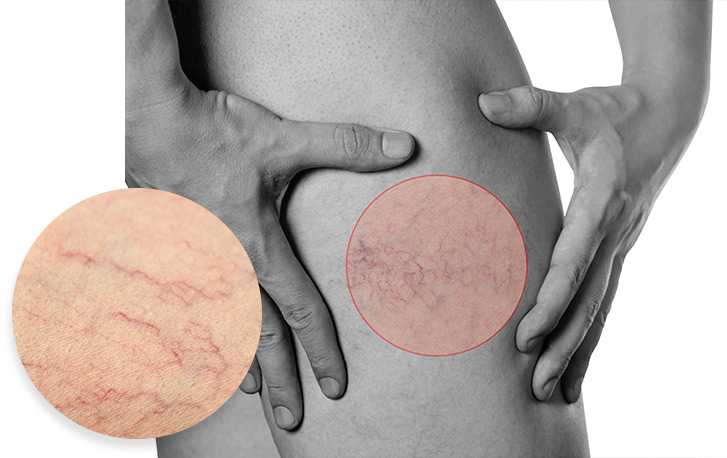
Spider veins, also called telangiectasis, are damaged blood vessels that appear as thin red, blue, or purple lines beneath the skin’s surface. They are common on the legs and face but can appear anywhere on the body.
Spider veins are a nuisance to the eye and can sometimes indicate underlying medical or circulatory problems. These web-like blemishes on your skin may have started as tiny spidery lines, but they can grow and widen over time.
Advanced Dermatology, P.C. offers several spider vein treatment options, like sclerotherapy and laser treatments, to remove unsightly spider veins, improve the appearance of your skin, and boost your confidence.


What Are Common Spider Vein Causes?
The circulatory system pumps the blood through the veins, delivering the nutrients and oxygen the organs need to function. Once the organs are nourished, they carry waste-rich blood back to the heart to receive more nutrients for dispersion.
Tiny, one-way valves within the veins ensure blood moves in the right direction. When blood is forced to flow upward against the force of gravity, as it does in the legs, these valves can malfunction. When they do, blood backs up inside your veins, resulting in the enlargement or ballooning of the veins.
Though spider veins and telangiectasia (dilated blood vessels) are part of the blood network, they are not essential to blood transportation. They can be safely eliminated with proper spider vein treatment.
The most common factors that contribute to the development of spider veins include:
- Genetics
- Physical trauma
- Illness
- Sun exposure
- Weight gain
- Nutrition
- Pregnancy
Other factors contributing to spider veins may include events that alter a person’s hormone balance or activities, hobbies, and professions that require standing or sitting for prolonged periods.
How Do Spider Veins Form?
The circulatory system pumps the blood throughout the body to deliver nutrients and oxygen that your organs need to function. Once your organs are nourished, your veins will carry the blood back to the heart to receive more nutrients for dispersion. When blood is forced to flow upward against the force of gravity, as it does in the legs, the one-way valves in your veins can malfunction. The blood backs up and causes spider veins and varicose veins in more severe cases.
Spider veins commonly arise on legs and faces, which is a cosmetic worry for many who have them. Genetics, physical trauma, illness, sun exposure, hormones, nutrition, and extended sitting or standing can cause spider veins. The American Society for Dermatologic Surgery informs us that most people will experience some vein malfunction throughout their lives. Women are more likely to develop spider veins due to hormones: over forty percent of women endure vein issues, with 4 out of 5 women having difficulties by the time they reach 80 years of age.
Where Do Spider Veins Commonly Appear?
Spider veins commonly arise on legs and faces but can appear anywhere on the body.
The American Society for Dermatologic Surgery tells us that most people will experience some vein malfunction throughout their lives. Women are more likely to develop spider veins due to hormones. Over 40% of women endure vein issues, with four out of five having difficulties by the time they reach 80.
Are Spider Veins Dangerous?
Typically, spider veins are not dangerous, but they can sometimes be an early warning sign of chronic vein insufficiency (CVI). CVI is a serious vein disease that can negatively impact your quality of life.
Like spider and varicose veins, CVI is caused by broken one-way vein valves in the legs. However, spider vein symptoms are usually painless and only include a slight itching or burning sensation, whereas CVI can cause dull aching, cramping, or a heavy feeling in the legs.

How To Fight Spider Veins
Here are five things you can start doing today to help fight spider veins:
- Sunscreen
Wear sunscreen to protect your skin from sun damage, premature aging, and skin cancer and help keep your circulatory system safe. SPF helps block damaging UV rays that promote spider vein formation. - Stretch out
Avoid crossing your legs at the knee. Crossing your legs disrupts blood flow, which can cause blood to pool and damage blood vessels. When your vein valves and walls are weakened, spider and varicose veins can take hold. - Move it
Keep your cardiovascular system healthy with regular exercise. To get the blood flowing, try to move around as much as possible during the day, taking leisurely strolls around the office if necessary. Avoid staying seated for more than 30 minutes at a time. - Raise them
Elevate your feet above your heart to help relieve blood pressure and encourage your blood to flow back toward the heart. Everyone deserves some relaxation time. When done correctly, it can help your veins as much as your mindset. - Step right
Leave your high heels at home and purchase a comfortable pair of flats or sneakers. No matter what you do, you need to make sure you’re doing it in the right shoes, and keeping the pressure off your feet can make a world of difference.
If you’re concerned about spider veins, powerful treatment options are available to minimize their impact. Contact Dr. Gallagher for a consultation and set yourself on the road to removing unsightly spider veins.

How to Get Rid of Spider Veins?
Advanced Dermatology, P.C. offers the following spider vein treatment options:
Sclerotherapy
Sclerotherapy is a nonsurgical spider vein removal procedure and is performed in our offices. After localizing and examining the dysfunctional veins or telangiectasia, the doctor will inject a chemical solution, called a sclerosant, into the blood vessel. The sclerosant displaces the blood in the vein, which will then collapse from the lack of blood and action of the sclerosant. Eventually, your body will absorb the collapsed vessel.
A typical sclerotherapy treatment lasts approximately 15 minutes. The number of injections or treatments depends on the extent of the vein/telangiectasia disorder and the type and concentration of solution used.
Some patients will notice immediate clearing of the veins, though some effects may not be seen for up to three months. Our doctors in Queens, Long Island, NY, Bergen County, NJ, and other locations will answer any questions that you may have during your recovery process.
Lasers
We can use lasers for spider vein treatment. Pulses of laser light beams are delivered to the targeted vein/telangiectasia. The heat from the lasers will ultimately cause the veins to dissolve or collapse depending on the laser, and your body will absorb the collapsed vessel.
With each laser treatment, the blood vessels close further. We sometimes utilize laser treatment in conjunction with sclerotherapy to achieve the best results.
For a couple of weeks, the area surrounding the treated veins (whether by laser or injection technique) may appear discolored or bruised. This is normal. For this reason, we usually suggest treating spider veins on legs at any time except during the summer.
Over time, the discoloration will fade. Your doctor may suggest wearing heavy-duty support hose or pressed bandages to help keep pressure on the veins and reduce bruising. Although strenuous activities should be avoided during treatment, daily activities should not be interrupted. Walking is encouraged to promote healing and lessen any risks.
While sclerotherapy or laser treatments do not prevent future spider veins, they can improve the appearance of your skin and give you the confidence you need to stop covering up and start showing off your younger, healthier-looking skin.

Can Large Veins Be Treated?
Treating large painful veins traditionally includes hospitalization, surgery, and extended recovery.
A simple office-based laser treatment, CoolTouch CTEV™, offers:
- Rapid relief of symptoms—virtually pain-free
- No downtime
- No general anesthesia
Patients experience very little bruising and fewer complications. They may quickly resume their normal activities, with an over 96% success rate.
Note: Most insurance plans cover this treatment Depending on your condition.
